Written by admin
Posted on: April 20, 2020
In the span of a month life as we knew it has changed. A microscopic virus has changed the fabric of our society. Social distancing, self-quarantine, PPE, distance learning, are now part of our everyday vocabulary. The disease is rapidly being understood, but only as hundreds of thousands are infected and tens of thousands have died. Why do some develop overwhelming lung inflammation? Why are there asymptomatic carriers? How long does one stay infectious after recovering? Is there immunity after being infected? The way out of this is difficult to see at times and understandable responses include anxiety, anger, sadness. Even all of these in the same day… same hour! The way out will undoubtably include more comprehensive testing, better treatments, and a vaccine.
MY INTRODUCTION TO COVID-19’s ARRIVAL
My interaction with the virus occurred early in Massachusetts’ involvement. I had a “medium risk” (as defined by the CDC) exposure on March 4th. When this patient’s test returned positive two days later, I immediately began a home quarantine. The medical community at that time believed you were likely only contagious if symptomatic and I did not separate from family (wife and 3 boys). We knew at that time from data out of China and Italy that average time from exposure to symptoms was 5 days and the range was 2-13 days. Knowing what we now know about the prevalence of asymptomatic (or minimally symptomatic) carriers I would have isolated in my basement.
That weekend my brain started to wrap around the nature of this virus, the threat it posed, the fear it was going to cause. Although I did not isolate from my family, we did keep the kids out of school and my wife did not work the week of March 9th. We all quarantined together. This was not so much to protect our kids, but rather to avoid the small risk that I might develop symptoms and to protect our community. The next week schools shut down. Thankfully I did remain unaffected. I did as much as I could to help care for my patients from home that week (before Governor Baker’s state of emergency expanded the use of telehealth.) On March 18th I returned to work to a new and still evolving world. There is still a lot to be learned about how this virus impacts cancer patients. There is some data for other countries that started before us that cancer patients may not me infected at high rates, but that the severity of infection might be worse. The American Society of Clinical Oncology (ASCO) has launched a COVID-19 in Oncology Registry,
https://www.asco.org/asco-coronavirus-information/coronavirus-registry?cid=DM4879&bid=41712109
Coordinated efforts like this will hopefully teach us more as time unfolds.
HOW HAS CANCER CARE CHANGED?
Protecting a vulnerable patient population
A patient with cancer is in a higher risk population, particularly those with active cancers and underdoing potential immunosuppressive treatments. Cancer Centers need to be an oasis where patients feel as safe as possible. This requires limiting foot-traffic to only those who really need to be in the building. Telehealth, which was struggling to find a niche in medicine, is now crucial for any routine follow up visits. One difficult decision was to limit all visitors. Caregivers are often the vital piece to the patients physical / emotional / metal support. But it is strictly an odds calculation. The fewer people that come into the building the more patients are protected. We utilize facetime and speakerphone functions to “get caregivers into the room” for visits, especially when there are treatment decisions being made.
Protecting health care providers
It is well documented the toll that the pandemic is having on health care workers. Our obligation is also to protect those providing the care. Again, in this regard, limiting visitors is important and using telehealth to keep foot-traffic down. Social distancing is adhered to as much as possible. We have always practiced hand hygiene but now doubling down on this. Wearing masks throughout our day. Utilizing zoom for our many internal meetings, cancer conferences, etc.
Treatment decisions
In cancer care COVID-19 has had a major impact on treatment decisions. It is a variable that is brought into the discussion. Elective surgeries are being postponed. One example is elective surgery for early stage, hormone positive breast cancer. Guidelines, such as from the American College of Surgeons now call for placing women on endocrine therapies to halt growth or even shrink tumors, while delaying surgery. https://www.facs.org/covid-19
This is a well-studied safe approach, but different from what would be standard during non-COVID-19 times and difficult to accept for a patient who just wants the tumor out asap. In cancers where there might be two options with equivalent outcomes we are certainly leaning toward oral / pill options that allow fewer visits to the cancer center and/or less immunosuppressive options. In situations where chemotherapy might offer small overall benefit, as in the 5-7% absolute survival benefit for stage II lung cancer after surgery, we are incorporating COVID-19 into the risk/benefit discussion.
Supporting mental / emotional health – for all involved
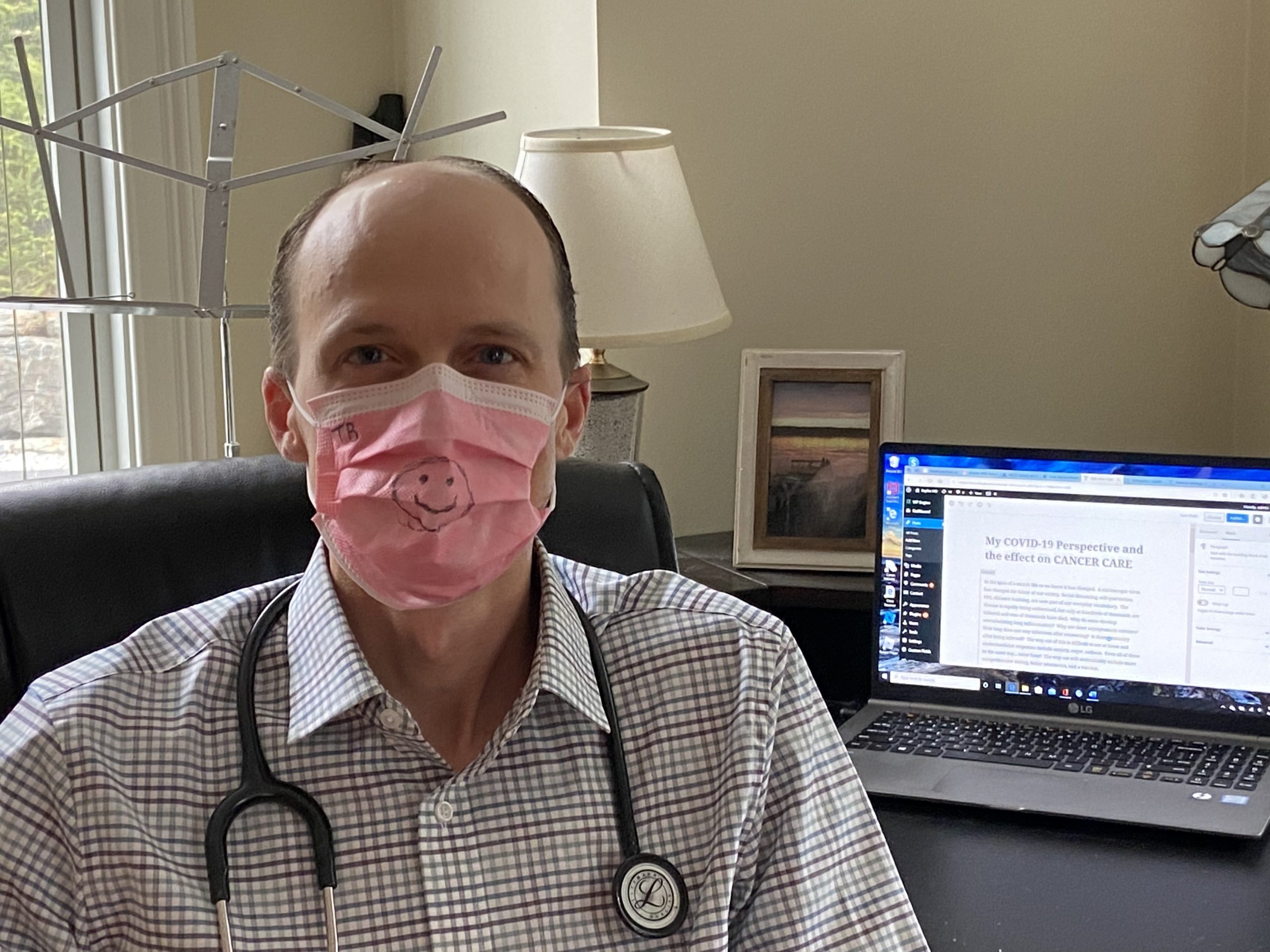
A cancer diagnosis is difficult enough. I have written about my experience with this extensively. It shatters your world, takes you off the rails of where you thought you were headed. If you are not one who has meditated on death, it forces that upon you. Now consider a cancer diagnosis in the setting of a global pandemic. New fears added into the mix include: having to come in and out of health care facilities at a time we are being told to socially distance, the fear that treatment will make one more susceptible to severe COVID-19 symptoms, not having a loved-one by your side for a difficult office visit / a first treatment because of no-visitor policies. An interesting challenge I read about recently is the loss of human connection / empathy / comfort when everyone is wearing masks. I have always felt that one of my strongest tools was a well-timed warm smile. I recently saw an article about health care providers in New York City wearing large laminated pictures of their smiling faces. A nurse in our office used a marker to draw a smiley face on her mask. I also think health care workers must be even more conscious about the tone of our voices and using replies that let the patient know we hear what they are saying. Utilizing the video portion of telehealth visits provides that “face to face” connection. At our Cancer Center we have our exercise classes up and running through zoom. Providing the outlet of movement and social support / connection to patients at home has been very well received. We have to be creative during this time to continue to support the whole patient, and caregiver, through a difficult journey during a difficult time.


Thank you for this informative and comforting information for cancer patients. It means a lot to hear from you during this pandemic. Treatment decisions are so important and questioning. My mind is at ease after reading your article.
I’m glad to hear, Caroline. Be well and talk to you soon!
Very informative Thank You, Dr. Bayless for all that you do!
Thank you so much for this wonderful article. Since the Moving Forward class was postponed
I am takibg part in a Zoom call with Viktoria Seavey every Saturday for the Intuitive Art class. I was not aware that the excercise class was also on Zoom. I will check it out. Be well and stay safe.
That’s great, Maureen. Definitely try out the zoom exercise class if you can!